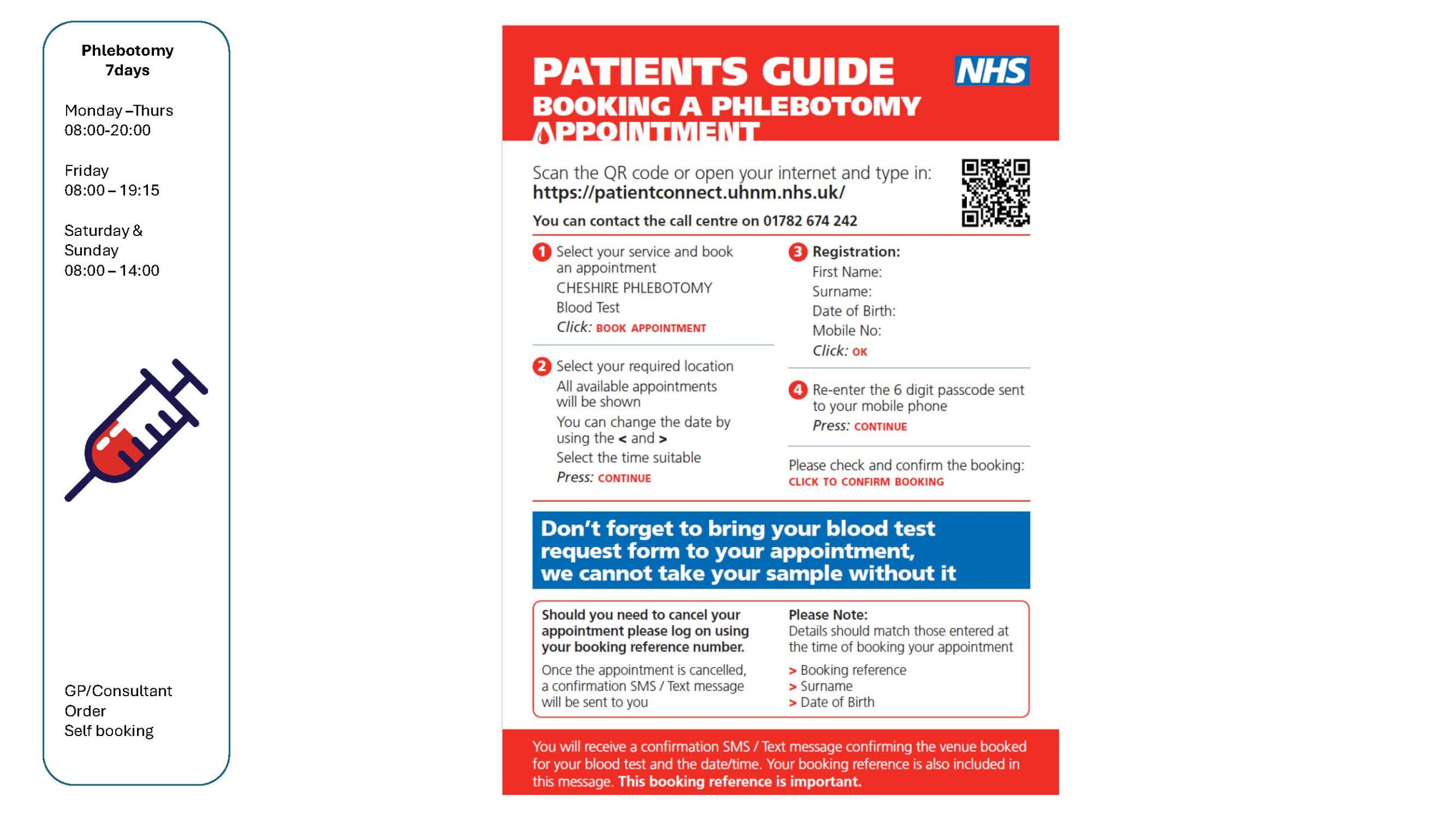
You can book your blood test by contacting the practice on 01606 544241 we have a phlebotomist clinic on a Tuesday morning or you can book a blood test online at another location.
Please ensure if you book your blood test online you have collected your blood form from the practice (if you have an appointment at another location without your blood form they will not be able to carry out the blood test)
If you would like to book a blood test at another location please use the following link https://patientconnect.uhnm.nhs.uk/booking/services
Blood tests have a wide range of uses and are one of the most common types of medical test.
For example, a blood test can be used to:
- assess your general state of health
- check if you have an infection
- see how well certain organs, such as the liver and kidneys, are working
- screen for certain genetic conditions
Most blood tests only take a few minutes to complete and are carried out at your GP surgery or local hospital by a doctor, nurse or phlebotomist (a specialist in taking blood samples).
Read about some common types of blood test.
For more information about a wider range of tests, search the blood test A-Z index on Lab Tests Online UK.
Preparing for a blood test
The healthcare professional who arranges your blood test will tell you whether there are any specific instructions you need to follow before your test.
For example, depending on the type of blood test, you may be asked to:
- avoid eating or drinking anything (fasting) apart from water, for up to 12 hours – read more about eating and drinking before having a blood test
- stop taking certain medicines
It’s important to follow the instructions you’re given, as it may affect the result of the test and mean it needs to be delayed or carried out again.
What happens during a blood test?
A blood test usually involves taking a blood sample from a blood vessel in your arm.
The arm is a convenient part of the body to use because it can be easily uncovered. The usual place for a sample to be taken from is the inside of the elbow or wrist, where the veins are relatively close to the surface.
Blood samples from children are often taken from the back of the hand. Their skin may be numbed with a special spray or cream before the sample is taken.
A tight band (tourniquet) is usually put around your upper arm. This squeezes the arm, temporarily slowing down the flow of blood and causing the vein to swell. This makes it easier for a sample to be taken.
Before taking the sample, the doctor or nurse may clean the area of skin with an antiseptic wipe.
A needle attached to a syringe or special container is inserted into the vein. The syringe is used to draw out a sample of your blood. You may feel a slight pricking or scratching sensation as the needle goes in, but it shouldn’t be painful. If you don’t like needles and blood, tell the person who is taking the sample so they can make you more comfortable.
When the sample has been taken, the tourniquet will be released, and the needle will be removed. Pressure is applied to the skin for a few minutes using a cotton-wool pad. A plaster may be put on the small wound to keep it clean.
After the test
Only a small amount of blood is taken during the test so you shouldn’t feel any significant after-effects.
However, some people feel dizzy and faint during and after the test. If this has happened to you in the past, tell the person carrying out the test so they’re aware and can help you feel more comfortable.
After the test, you may have a small bruise where the needle went in. Bruises can be painful, but are usually harmless and fade over the next few days.
Blood test results
After the blood sample has been taken, it will be put into a bottle and labelled with your name and details. It will then be sent to a laboratory where it will be examined under a microscope or tested with chemicals, depending on what’s being checked.
The results are sent back to the hospital or to your GP. Some test results will be ready the same day or a few days later, although others may not be available for a few weeks. You’ll be told when your results will be ready and how you’ll be given them.
Sometimes, receiving results can be stressful and upsetting. If you’re worried about the outcome of a test, you may choose to take a trusted friend or relative with you. For some tests, such as HIV, you will be offered specialist counselling to help you deal with your results.
